[This is the continuation of the post from last week.]
To speak of an “Anthropocene for pathogens” is to imagine the ways that human transformation of the environment has shaped the ecology and evolution of infectious microbes. In other words, it is to imagine the interrelated history of humans and our germs.
 Many people are familiar with a model of disease history presented in Jared Diamond’s Guns, Germs, and Steel and which, in no small part, goes back to William McNeill’s Plagues and Peoples. In this model, the domestication of animals was the major turning point in the long relationship between humanity and pathogens. Then, the rise of large, densely-packed urban areas allowed the evolution of “crowd diseases,” infections that required large populations to be sustained. Cultures across Eurasia were said to have developed some level of immunity to these pathogens and then to have unleashed devastation with the colonization of the New World.
Many people are familiar with a model of disease history presented in Jared Diamond’s Guns, Germs, and Steel and which, in no small part, goes back to William McNeill’s Plagues and Peoples. In this model, the domestication of animals was the major turning point in the long relationship between humanity and pathogens. Then, the rise of large, densely-packed urban areas allowed the evolution of “crowd diseases,” infections that required large populations to be sustained. Cultures across Eurasia were said to have developed some level of immunity to these pathogens and then to have unleashed devastation with the colonization of the New World.
This model has started to break down in the face of genomic evidence. First, domesticated animals have not been a crucially important source of novel human pathogens. While some germs probably did evolve from farm animals (notably measles, which diverged from an ancestral Rinderpest virus though only sometime in the first millennium), it turns out that wild animals have been a far more important and enduring source of dangerous emerging diseases. Second, the role of immunity in the story is often unclear. If Eurasian populations evolved superior innate immunity to specific pathogens, clear examples are notably lacking, despite no lack of searching. The idea that Europeans introduced germs to which they had evolved resistance onto “virgin populations” also understates the role of other factors in shaping the health dimensions of New World expansion. Third, the old model actually underestimates the role of geography in shaping disease ecologies and the ways that humans have configured and connected different ecologies. John McNeill’s work on the spread of malaria and Yellow Fever into the Caribbean exemplifies what is possible when history, geography, ecology, and evolution are interwoven.
In short, the old model of disease history is crumbling and nothing has yet replaced it, in part because the rise of genomic evidence is moving more quickly than the field can keep up. But, ultimately, the story of human pathogens will be one that requires us to imagine how humans have shaped their ecology and evolution. It will be a story that is temporally deep, global in scale, and sensitive to the importance of geography. Already we might try to catalogue some of the ways that human civilization has changed the rules of the game for infectious microbes.
Human Habitats Define Germ Habitats
- WASTE DISPOSAL. The built environment for humans is also the built environment for our invisible co-residents. The ecologies created by humans living in small, ambulatory, foraging bands were radically different from the ecologies created by humans living in giant, stationary, agriculturally provisioned cities. The rise of farming, followed by the rise of urban habitats, created, as Gillings and Paulsen suggest, the Paleoanthropocene. Among the more important consequences, cities have been a boon for microbes dependent on the fecal-oral route. Bacteria like Shigella and Salmonella typhi, and viruses like rotaviruses, flourish in environments where excrement finds its way into food and water supplies.
 Even today, clean water is arguably the most important health resource of all, and for thousands of years, human cities have been conducive environments for pathogens. In coming years, with the recovery of more ancient genomic evidence, it will be interesting to see if and how these common pathogens underwent adaptive genetic evolution in response to new environments created by human social development.
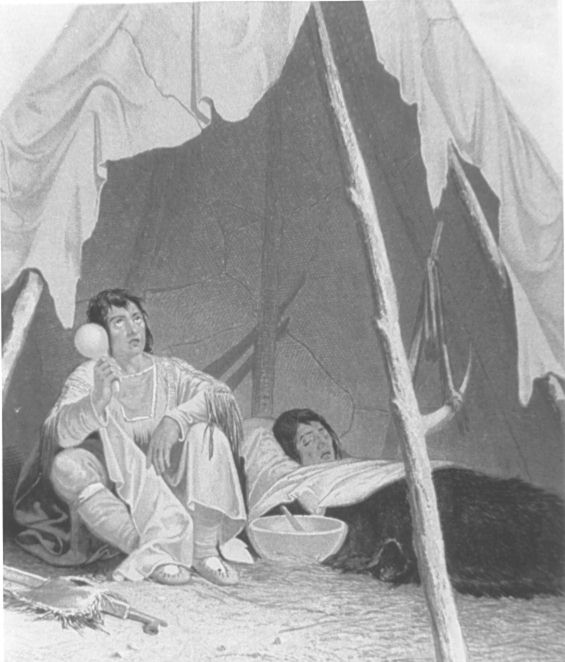
Even today, clean water is arguably the most important health resource of all, and for thousands of years, human cities have been conducive environments for pathogens. In coming years, with the recovery of more ancient genomic evidence, it will be interesting to see if and how these common pathogens underwent adaptive genetic evolution in response to new environments created by human social development.  DENSITY. Many common bacteria and viruses (from the common cold to more dangerous enemies like measles) are transmitted directly between humans via aerial droplet, saliva, blood, or sexual contact. Large human populations living closely together created unprecedented opportunities for virulent pathogens. The growth of cities was a prerequisite for the establishment of some germs as obligate human pathogens. Smallpox and measles require high population densities to maintain a chain of continuous transmission. Both of these viruses emerged from animal diseases (an ancestral rodent Orthopoxvirus in the case of smallpox, and a cattle disease related to Rinderpest virus in the instance of measles). Over the course of human history, there were probably extremely virulent pathogens that emerged but quickly burned themselves out by killing too many victims, too quickly, and running out of new susceptible hosts.
DENSITY. Many common bacteria and viruses (from the common cold to more dangerous enemies like measles) are transmitted directly between humans via aerial droplet, saliva, blood, or sexual contact. Large human populations living closely together created unprecedented opportunities for virulent pathogens. The growth of cities was a prerequisite for the establishment of some germs as obligate human pathogens. Smallpox and measles require high population densities to maintain a chain of continuous transmission. Both of these viruses emerged from animal diseases (an ancestral rodent Orthopoxvirus in the case of smallpox, and a cattle disease related to Rinderpest virus in the instance of measles). Over the course of human history, there were probably extremely virulent pathogens that emerged but quickly burned themselves out by killing too many victims, too quickly, and running out of new susceptible hosts.
Humans Transform Ecologies for Hosts and Vectors
- ZOONOTIC DISEASE. Many diseases capable of infecting humans are not actually human diseases, and most new human diseases evolve from animal diseases. There has probably been too much emphasis on the importance of animal domestication, per se, as a major driver of human disease evolution; in fact, genomic evidence is revealing that farm animals account for relatively few human pathogens, and in fact in some cases – like tuberculosis – it seems that human farmers got their livestock sick, rather than vice versa.
 More importantly, we have learned that wild animals like rodents, bats, and primates are especially important reservoirs of zoonotic diseases and sources of emerging human infections. Human occupation of the planet has changed the ecological setting for other animals that play crucial roles in pathogen evolution and transmission. Most notoriously, the three great global pandemics of bubonic plague, Yersinia pestis, required an elaborate ecological platform, dependent on human networks and commensal rodents.
More importantly, we have learned that wild animals like rodents, bats, and primates are especially important reservoirs of zoonotic diseases and sources of emerging human infections. Human occupation of the planet has changed the ecological setting for other animals that play crucial roles in pathogen evolution and transmission. Most notoriously, the three great global pandemics of bubonic plague, Yersinia pestis, required an elaborate ecological platform, dependent on human networks and commensal rodents.  VECTOR-BORNE DISEASES, like the scourge of malaria, depend on intermediaries such as ticks and mosquitos for transmission. Human occupation of the planet has and continues to modify the environment for vectors and therefore the pathogens they carry. The spread of the tick-borne Lyme disease in the northeastern US, still imperfectly understood, is almost certainly due to the spread of human suburban settlements and the unintended effects on populations of deer and white-footed mice. In much deeper historical time, the spread of falciparum malaria depended on the dispersal of the Anopheles Still today, Aedes mosquitos that carry dangerous viruses like those that cause Dengue Fever, Yellow Fever, and Chikungunya, are evolving in response to the opportunities presented by human habitats.
VECTOR-BORNE DISEASES, like the scourge of malaria, depend on intermediaries such as ticks and mosquitos for transmission. Human occupation of the planet has and continues to modify the environment for vectors and therefore the pathogens they carry. The spread of the tick-borne Lyme disease in the northeastern US, still imperfectly understood, is almost certainly due to the spread of human suburban settlements and the unintended effects on populations of deer and white-footed mice. In much deeper historical time, the spread of falciparum malaria depended on the dispersal of the Anopheles Still today, Aedes mosquitos that carry dangerous viruses like those that cause Dengue Fever, Yellow Fever, and Chikungunya, are evolving in response to the opportunities presented by human habitats.
Humans Transform Biogeography
- CONNECTIVITY. The Antonine Plague (discussed in Part I) was the first true “pandemic,” a disease event stretching across continents. It was made possible by the networks of trade and travel that linked different human populations in the late Iron Age. The steady advance
 of transportation technologies over the millennia has turned once separate human societies into more closely interconnected populations full of potentially susceptible hosts for human pathogens. Further, over the millennia, humans have introduced species far beyond their original geographic range and facilitated biological invasions. Genomic evidence is continuing to illuminate the dispersal of pathogens across the oceans in the wake of human expansion. Hepatitus C Virus, for example, seems to have originated in Africa in the early modern period and to have dispersed outward with the Atlantic slave trade.
of transportation technologies over the millennia has turned once separate human societies into more closely interconnected populations full of potentially susceptible hosts for human pathogens. Further, over the millennia, humans have introduced species far beyond their original geographic range and facilitated biological invasions. Genomic evidence is continuing to illuminate the dispersal of pathogens across the oceans in the wake of human expansion. Hepatitus C Virus, for example, seems to have originated in Africa in the early modern period and to have dispersed outward with the Atlantic slave trade. - CLIMATE CHANGE, increasingly driven by greenhouse gas emissions, impacts the geographic range and distribution of ecologically sensitive pathogens. Even before the onset of anthropogenic climate change, natural climate change and variability has been a major force in the dynamics of infectious diseases. Both of the major historic plague pandemics, for instance, seem to have had a climate trigger. The relationship between climate change and pathogen evolution is complex and unpredictable, but the health risks of climate change remain one of the more underappreciated dangers of the Anthropocene.
Human Health Is a War on Pathogenic Microbes
- IMMUNITY. Humans and pathogens have been battling since long before we were human. Given that infectious disease has been one of if not the main cause of death for a large part of the human past, it is unsurprising that pathogens have been a primary selection pressure on the human genome. Indeed it seems that pathogens have continued to shape the human genome even into the recent past. And it is also probable that pathogens have adapted and continue to adapt in response to the human immune system. In that sense, humans exert evolutionary pressure on microbes.
- THE EXTENDED IMMUNE SYSTEM. Maybe the single greatest change in the human experience has been the decline of mortality over the last two hundred years. Everywhere in the developed world, life expectancy has climbed from ca. 25-35 years to ca. 75 years or more. Most of this
 mortality decline is due directly to the conquest of infectious disease. The basic ingredients here are relatively well understood: (1) better nutrition; (2) public health, i.e. sanitation, hygiene, clean water, vector control, etc.; and (3) antibiotic pharmaceuticals. We could imagine all of these as part of an “extended immune system,” as humans have carried the molecular war against dangerous microbes to many fronts and achieved a fragile control over our ancient enemies. But of course evolution is relentless, and the spread of resistance against the small array of antibiotic weapons we have at our disposal is one of the great threats on the horizon.
mortality decline is due directly to the conquest of infectious disease. The basic ingredients here are relatively well understood: (1) better nutrition; (2) public health, i.e. sanitation, hygiene, clean water, vector control, etc.; and (3) antibiotic pharmaceuticals. We could imagine all of these as part of an “extended immune system,” as humans have carried the molecular war against dangerous microbes to many fronts and achieved a fragile control over our ancient enemies. But of course evolution is relentless, and the spread of resistance against the small array of antibiotic weapons we have at our disposal is one of the great threats on the horizon.
In short, humans have transformed the global environment for germs, and the biogeography of pathogenic microbes is an artifact of human history. If we could somehow recreate the World Health Organization map of global infectious disease
 risk (shown at the end of Part 1) for the year 1750, at the cusp of the Industrial Revolution, or the year 1, in the expanding Roman Empire, or the year 3000 BC, at the dawn of the Bronze Age, or the year 10,000 BC, at the origins of the Neolithic, the map would look very different in every case. To imagine these maps is to sense the importance of the Anthropocene for the pathogens whose evolution, dispersal, and demise our species has helped to engineer, often unintentionally. The shadow of the past hangs over the biology and biogeography of the microbial world that we have helped to create, and that is why I hope that historians will join forces with scientists to deepen our understanding of the planet that humans have made.
risk (shown at the end of Part 1) for the year 1750, at the cusp of the Industrial Revolution, or the year 1, in the expanding Roman Empire, or the year 3000 BC, at the dawn of the Bronze Age, or the year 10,000 BC, at the origins of the Neolithic, the map would look very different in every case. To imagine these maps is to sense the importance of the Anthropocene for the pathogens whose evolution, dispersal, and demise our species has helped to engineer, often unintentionally. The shadow of the past hangs over the biology and biogeography of the microbial world that we have helped to create, and that is why I hope that historians will join forces with scientists to deepen our understanding of the planet that humans have made.
This interesting piece just came out in the journal Science. It draws a vivid connection between ancient Rome and present-day Madagascar. “As cities burgeon and populations become more mobile, once-isolated diseases are increasingly likely to reach cities, where they can race out of control. “Next time,” Bertherat says, “we need to be ready to manage [plague] in an urban setting.””
http://science.sciencemag.org/content/358/6362/430.full
Fascinating stuff! I completely agree about the role of wild and domestic animals in zoonotic disease. But I do think antibiotic use in livestock is leading to increases in antibiotic resistant bacteria in general, which is a concern (I suppose we could file that under our “extended immune system”). But, like many of the issues you raised, I think there are still a lot of unknowns here:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3234384/